Atlantic Reproductive Medicine is now Atlantic Fertility. Learn more about the rebrand →
Male Fertility
Fertility Treatments
Fertility Basics
Are Vasectomies Reversible?
Understand how vasectomy reversal can restore fertility and when it’s effective.

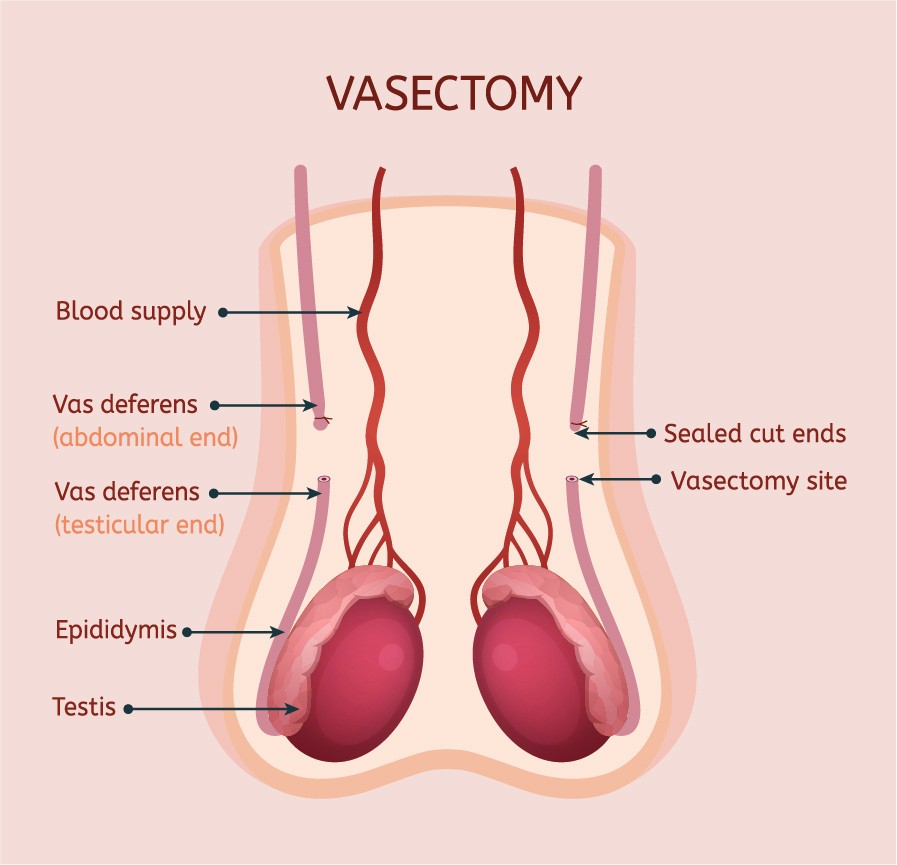
A vasectomy is an effective form of birth control that surgically blocks sperm from traveling up the vas deferens, tubes that carry sperm from the testicles to the urethra. This surgical procedure prevents sperm from mixing with the semen that is ejaculated into a woman’s vagina during intercourse.
For men who want to reverse their vasectomy, there is very good news: in almost all cases, vasectomies can be reversed. There are several reasons a man or a couple may desire a vasectomy reversal. A couple might change their mind about having additional children. A man might enter a new relationship and want to have children with his new partner. A younger man may simply have regrets about his vasectomy and want to reverse it so he can potentially have a family in the future.
What is a vasectomy reversal?
A vasectomy reversal is a surgical procedure that involves reconnecting the severed ends of the vas deferens to restore the flow of sperm in men who have previously undergone a vasectomy.
The most important factor determining reversal success is the experience of the surgeon. Your surgeon should be a fellowship-trained reproductive urologist who can perform both vasovasostomy (VV) and epididymovasostomy (EV). Your experienced surgeon should use a powerful operating microscope to magnify the vas deferens during your microsurgery.
A skilled surgeon can reverse vasectomy on most men regardless of the time elapsed since the surgery, even if that time is significantly longer than 10 years.
How Are Vasectomies Reversible?
During the surgical procedure, your surgeon will either reconnect the severed ends of your vas deferens or bypass a more complex blockage in order to restore sperm flow. A reversal is typically performed under general anesthesia and may take approximately four hours to complete. After a successful vasectomy reversal, sperm will again be able to travel from the testicles and be present in your semen.
A surgeon will typically reconnect the two ends of the vas deferens using one of these two reversal procedures:
Vasovasostomy (VV): This is the most common technique used for vasectomy reversal. The procedure involves making a small incision in the scrotum to access the severed ends of the vas deferens. The surgeon then removes any scar tissue or blockages in the vas deferens and reconnects the two ends of the vas deferens with sutures.
Epididymovasostomy (EV): This more complex technique involves attaching the vas deferens directly to the small organ (the epididymis) at the back of each testicle that holds sperm. This technique is also called vasoepididymostomy by some doctors.
An epididymovasostomy (EV) is more complicated than a vasovasostomy (VV). For various surgical reasons, an EV is generally only chosen by the surgeon if a vasovasostomy cannot be done.
A surgeon’s decision depends on whether sperm are seen when fluid from the vas deferens is analyzed during the surgery. Up to ten years with a vasectomy, a VV is more common, and after 10 years, an EV becomes more common. For this reason, a surgeon decides which of the two procedures is needed during the surgery, but the most important factor in determining whether sperm are found in the fluid during surgery is the length of time of having the vasectomy (the “vasectomy interval”). Oftentimes a combination of both procedures is required, especially if the vasectomy interval is around 10 years. For example, sometimes a vasovasostomy is needed on one side, and an epididymovasostomy is required for the other.
How Successful are VV and EV Surgeries?
A VV is successful 90-95% of the time, and an EV is successful approximately 50% of the time. Because the result can be bilateral VV, VV/EV, or bilateral EV, the success of the reversal to have sperm back to the ejaculate ranges from 50 to 95% and depends primarily on the type of reconstruction, which depends on the vasectomy interval.
Pregnancy rates which are separate from these figures range from around 30-90%, and success rates depend on age and fertility of the female partner as well.
Should Sperm be Banked During Vasectomy Reversal?
Many patients decide to cryopreserve (bank) their sperm as part of their vasectomy reversal. This is achieved by having a testicular sperm extraction (TESE) done at the time of the reversal surgery.
A TESE is a recommended procedure because up to5% of vasectomy reversals are unsuccessful (and up to 50%, in the case of bilateral EV, which is much less common). Therefore, it is smart to consider a TESE at the time of a vasectomy reversal surgery. Your surgeon will present this option to you when discussing your vasectomy reversal.
Are All Vasectomies Reversible?
Almost all vasectomies can be reversed according to the American Urological Association. In a few cases, there may be unique challenges. For example, if the vasectomy was done while fixing a hernia in the groin, it may not be as easy to join the ends of the vas deferens. In rare incidences, the ends of the vas deferens may not be able to be joined if an unusually long piece of the tube was removed during the vasectomy or if anatomy was previously altered from other prior surgery.
Once a vasectomy reversal is performed, it will take time for the sperm to reappear in the semen in significant numbers. Typically, it takes several months for the sperm count to return to pre-vasectomy levels. It is also important to note that while vasectomy reversal can restore fertility, it does not guarantee a pregnancy.
How Successful are Vasectomy Reversals?
Pregnancy rates after vasectomy reversal can range from about 30% to over 90% according to the Mayo Clinic. Success depends on many different variables: the type of vasectomy reversal procedure used, the experience of the surgeon, the partner’s age and fertility, the time since the original vasectomy, and whether the male had fertility issues before the initial vasectomy.
According to the Urology Care Foundation, it may take up to four months to a year for your partner to get pregnant after vasectomy reversal. Some women get pregnant in the first few months, while others may take years to conceive after the surgical procedure. Unless pregnancy is achieved shortly after the reversal, your doctor may want to check your semen quality periodically.

Confirming Vasectomy Reversal Success
Approximately 6-8 weeks after vasectomy reversal surgery, your surgeon will examine your semen under a microscope to see if sperm is present. When surgery is successful, sperm typically appear in the semen within a few weeks. It can take 4-6 months for the semen quality to stabilize, but increases occur for up to a year. However, if a bilateral epididymovasostomy is necessary, the appearance of sperm can be very delayed and can sometimes take a year or more to occur. Unless a pregnancy occurs, the only way to tell if a male’s vasectomy reversal was successful is to check the semen. Therefore, multiple semen analyses may need to be done over time.
Even if a vasectomy reversal is successful, achieving pregnancy depends on various factors, including the number and quality of the sperm present in semen and the female partner’s own fertility and age.
The Atlantic Fertility Difference
While vasectomy reversal is a viable option for couples who want to conceive after a vasectomy, it is important to understand the risks, benefits, and alternatives with a qualified healthcare provider before deciding to undergo the procedure.
At Atlantic Fertility in Raleigh, NC, Dr. Matt Coward is a highly experienced microsurgeon with over 10 years of experience performing vasovasostomy (VV) and epididymovasostomy (EV) vasectomy reversals using an operating microscope.
Vasectomy reversals are performed on-site with anesthesia in our fully equipped male fertility operating room outfitted with a state-of-the-art operating microscope. The operating room is adjacent to the andrology and embryology lab, where sperm can be cryopreserved (banked) on-site during the procedure.
If you are interested in a vasectomy reversal from one of the top urologists and male microsurgeons in the region, call Atlantic Fertility for a consultation at (919) 248-8777.
Reach out. Learn more.
A consultation at Atlantic Fertility gives you full-spectrum expertise for both female and male fertility—so you can understand your options and move forward with confidence.
