Azoospermia and Abnormal Semen Quality
What are azoospermia and abnormal semen quality?
Azoospermia is the medical term for the absence of sperm in the ejaculate.
Abnormal semen quality in a man’s ejaculate refers to quality issues with sperm in the semen that can make the sperm unable to achieve fertilization of an egg.
These conditions are not uncommon and are frequently the reasons for male infertility. Approximately 10% of infertile men and 1% of all men have azoospermia. Imagine a stadium filled with 50,000 men — approximately 5,000 to 7,500 will have infertility, and 500 will be azoospermic.
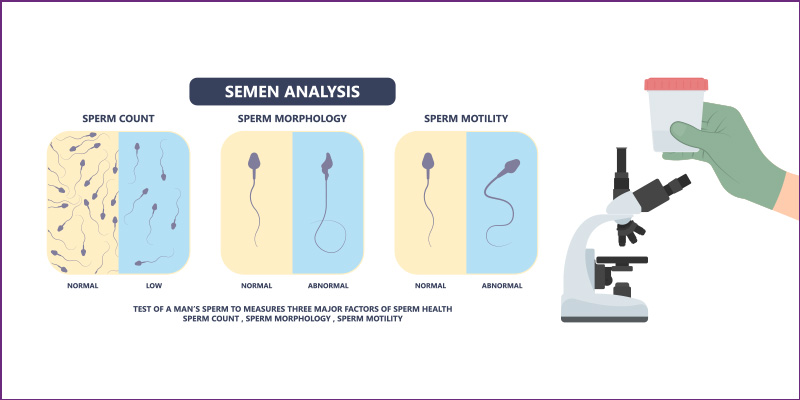
Since sperm health depends on various factors, including quantity, movement, and structure, abnormal semen quality is fairly common among men. A semen analysis helps determine if and how male factors may contribute to a couple’s infertility. It is important to keep in mind that an abnormal semen analysis does not mean that a man cannot father children. It just might take longer or require some medical assistance.
There are many viable solutions for both azoospermia and abnormal semen quality.
 “Finding out you have azoospermia or abnormal semen quality is a disappointing moment for my patients. But I am here with you to do everything I can to find solutions to achieving fertility. And there are many. I am with my patients every step of the way.” – Matt Coward, MD
“Finding out you have azoospermia or abnormal semen quality is a disappointing moment for my patients. But I am here with you to do everything I can to find solutions to achieving fertility. And there are many. I am with my patients every step of the way.” – Matt Coward, MD

ON THIS PAGE
The first step in addressing infertility concerns is for both partners to undergo fertility testing, physical exams, and medical history analysis to determine the problems and possible solutions.
Infertility is an increasing trend. In the United States, one in eight couples experiences infertility. Among heterosexual women aged 15 to 49 years with no prior births, about 1 in 5 (19%) cannot get pregnant after one year of trying (the definition of infertility). Half the time, couple infertility is due to a malefactor, and half the time, to a female factor. Exploring the fertility of both partners increases the odds of finding the best solutions for the couple.
Semen samples can provide answers to infertility issues
For males, a semen sample is typically one of the first steps to uncovering potential reasons for a couple’s infertility. The male provides a semen sample in a sterile cup. It is examined under a microscope for count, shape, and mobility. More than one sample is provided and examined, as different days can produce different results.
How are semen samples obtained?
Semen samples are typically obtained via masturbation by ejaculating into a special container in a private room at the doctor’s office. If you prefer an alternative method of semen collection, such as collection at home, your sample must be brought in for analysis within one hour of collection. Most specialist offices, including ours, prefer that the sample be collected in the office to ensure optimal conditions.
What causes low semen volume?
One of the most common causes of semen volume is incomplete or improper collection of a sperm sample. Sperm quality can also fluctuate. For these reasons, most specialists gather two or more semen samples on different days to ensure consistency between the samples.
To ensure the best possible accuracy in a collection, you will be asked to:
- Make sure all semen gets into the collection
- Abstain from ejaculating for two to five days before collecting a sample
- Avoid the use of lubricants which can affect sperm motility
- Collect a second sample at least two weeks after the first sample

How is sperm counted?
Male sperm are produced continually in the testicles and take 74 days on average from production to ejaculation. A semen analysis, therefore, reflects the sperm quality from three months prior. The sperm count and motility are determined by counting how many sperm appear within squares on a grid pattern under a microscope.
What is considered a low sperm count?
Average sperm densities in an ejaculate are approximately 75 million per milliliter. If there is fewer than 15 million sperm per milliliter or less than 39 million sperm total per ejaculate, the sperm count is considered low.
Some men with low sperm counts can successfully father children. And some men with normal sperm counts are unable to father children. There are many factors involved in reproduction, and the number of sperm in your semen is only one. Even if you have enough sperm, other factors are important to achieve a pregnancy, including normal sperm movement (motility).
If your semen analysis indicates azoospermia or abnormal semen quality, your specialist begins to analyze the possible causes.
Obstructive vs. Nonobstructive Azoospermia
The causes of azoospermia can be “obstructive,” meaning there is an anatomical blockage preventing sperm from entering the ejaculate, or it can be “nonobstructive,” meaning the lack of sperm is due to decreased sperm production by the testis. The testis could be making sperm, but the amount may not be enough to have a noticeable amount come out in the ejaculate.
What causes azoospermia?
There are several potential causes of azoospermia. These include medical treatments such as chemotherapy, radiation, or environmental toxins; some genetic conditions such as Klinefelter’s syndrome; poor testicular development as a fetus/child; and some anatomical abnormalities such as varicoceles or the absence of the vas deferens. The use of some recreational drugs, such as narcotics, cannabis, or alcohol, can sometimes cause azoospermia. And then there is the most obvious cause: vasectomy, which prevents sperm from joining other fluids in the ejaculate. The good news is that most vasectomies can be reversed.
Tests to determine the cause of low sperm count or azoospermia
Your infertility specialist will begin exploring potential reasons for azoospermia with a physical examination of your genitals and asking questions about any inherited conditions, illnesses, chronic health problems, injuries, surgeries, sexual development and habits, and any other factors that could affect your sperm count.
Other tests your specialist might recommend include:
- Scrotal ultrasound. This exam uses high-frequency sound waves to examine your testicles and supporting structures.
- Post-ejaculation urinalysis. Sperm in your urine can indicate your sperm are traveling backward into the bladder instead of out your penis during ejaculation (retrograde ejaculation).
- Transrectal ultrasound. A small, lubricated wand is inserted into your rectum to check your prostate and check for blockages of the tubes that carry semen (ejaculatory ducts and seminal vesicles).
- Hormone testing. A blood test can be done to determine the level of hormones produced by your pituitary gland and testicles, both of which play a key role in sexual development and sperm production.
- Genetic tests. A blood test can reveal whether your Y chromosome has any genetic abnormalities. Genetic testing can also be ordered to diagnose various inherited or congenital syndromes.
- Specialized sperm function tests. Sperm DNA fragmentation is a test that determines the DNA health of the sperm.
- Testicular biopsy. A biopsy can remove samples from the testicle to determine if sperm production is normal. A biopsy is typically only used in certain situations.
In the past, almost all men with azoospermia underwent a biopsy to distinguish obstructive from non-obstructive causes and to get an accurate and specific diagnosis. But in modern practice, a biopsy is rarely necessary.
In most cases, specialists can accurately determine whether or not a man has an obstruction causing azoospermia. Different areas of the testis might show different patterns of nonobstructive azoospermia. For example, one area might show decreased production of mature sperm (hypo spermatogenesis or maturation arrest). Another area might show the absence of sperm precursor cells (Sertoli-cell-only syndrome).
Doing a diagnostic biopsy does not often change the ultimate management for men with nonobstructive azoospermia, which is why biopsies are only done now in rarer cases. A nonobstructive cause is often treated with microdissection testicular extraction (microTESE), which offers one of the best chances of locating sperm for assisted reproductive techniques (ART). Sometimes, during microTESE, a tiny specimen will be sent for pathological evaluation.
Treatments for abnormal semen quality or azoospermia
Treatments for low sperm count or azoospermia include:
- Vasectomy reversal: Prior vasectomies can be reversed in many cases.
- Surgery. Surgery can correct varicocele or repair obstructed vas deferens. In cases where no sperm are present in the ejaculate, sperm retrieval techniques can retrieve sperm directly from the testicles or epididymis.
- Hormone treatments and medications. Hormone replacement or medications can be used in cases where infertility is caused by high or low levels of certain hormones or problems with how your body uses and responds to hormones.
- Infection treatments. Antibiotics are used to cure an infection of the reproductive tract. However, this does not guarantee that fertility will be restored.
- Treatments for sexual intercourse problems. Medication or sexual counseling might be recommended to improve fertility in conditions such as premature ejaculation or erectile dysfunction.
- Assisted reproductive technology (ART). ART treatments may involve obtaining sperm through normal ejaculation, surgical extraction, or from donor individuals, depending on your particular circumstances. Sperm is then inserted into the female genital tract or used for IVF or intracytoplasmic sperm injection.
The Atlantic Difference
Each semen analysis is unique. If you have an abnormal semen analysis or azoospermia, your fertility specialists at Atlantic Reproductive Medicine will discuss all potential tests, treatments, and solutions for achieving fertility. We will ensure you are fully informed and making the best decisions for you and your unique situation.
Contact us if you are concerned about infertility and have questions @ (919) 248-8777.
