
INVOcell
A Potentially Cost-Saving Option for Fertility Patients
The cost of fertility treatment can be a barrier between patients and their plans for a family. The INVOcell, an FDA-approved gas-permeable vaginal culture device, allows patients to incubate eggs and sperm themselves, decreasing costs and increasing access to fertility treatment. Atlantic Reproductive Medicine is happy to be the first practice in the Raleigh area that offers intravaginal culture with INVOcell in the hope that this treatment will allow more patients to afford fertility care.
Traditional IVF vs. INVOcell
The IVF laboratory is an intensive care unit for embryos. It requires air filtration systems, incubators with continuous monitoring and alarm systems, and highly trained embryologists to care for eggs, sperm, and embryos outside the body for five to six days of embryo culture. Intravaginal culture can potentially decrease treatment costs by reducing the need for laboratory and embryologist intervention.
The ovarian stimulation for IVF involves taking medications to recruit multiple eggs so that patients have the best return upon their investment. Robust ovarian stimulation requires many ultrasound and blood tests to monitor the ovarian response. These factors add to the expense of IVF. With INVOcell, we use a more modest ovarian stimulation requiring less medication and monitoring, which provides another cost savings over traditional IVF.
How INVOcell Works
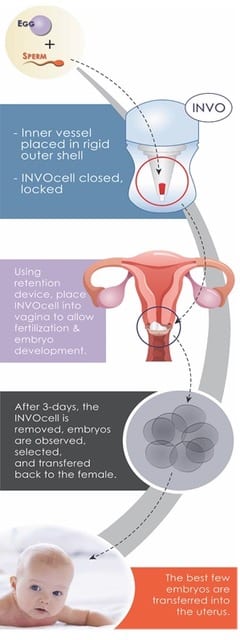
The INVOcell is a small device made of plastic that is permeable to gases, allowing eggs, sperm, and embryos to develop inside the vagina. Eggs are first retrieved and then mixed with sperm in the laboratory for a few minutes. Next, eggs are loaded into the culture media in the INVOcell device and placed into the vagina. Because the plastic is permeable to gases and because the gas mixture and temperature at the top of the vagina are similar to the gas mixture and temperature inside the fallopian tube, a patient can use their own body, rather than the IVF lab, to simulate the necessary conditions for the eggs, sperm, and embryos to develop.
After five days, the device is removed from the vagina, and the embryos are removed from the device. The best-quality embryo or embryos are transferred into the patient’s uterus, and any additional high-quality embryos are frozen for future use.
While INVOcell is a useful fertility tool, it should not be considered a replacement for traditional IVF. When used in a group of patients predicted to have high chances of success with IVF (37 or younger, body mass index less than 36, normal ovarian reserve, and good sperm parameters), INVOcell generated fewer top-quality blastocysts than traditional IVF. Because only one or two embryos were needed for transfer, the birth rates were similar (55% for INVOcell compared to 60% for traditional IVF). However, the INVOcell patients had fewer embryos to freeze.
INVOcell also requires sperm that are functional enough to fertilize eggs without assistance in the device. Patients with certain abnormal sperm parameters should undergo traditional IVF with intracytoplasmic sperm injection (ICSI) rather than INVOcell culture.
INVOcell vs. Intrauterine Insemination (IUI)
For some patients, the higher pregnancy rate of INVOcell may make it an attractive replacement for IUI. One in four couples with infertility conceive with up to three cycles of intrauterine insemination. In the study of INVOcell, just over half of patients conceived in one cycle, and some had embryos to freeze for future use. The cost of INVOcell is slightly greater than the cost of three cycles of IUI and approximately half of the cost of traditional IVF, so some couples may elect to skip IUI and go directly to INVOcell.
The promising published success rates for INVOcell were from a group of patients with infertility predicted to have good chances of success with IVF (37 years of age or younger, normal ovarian reserve, good sperm parameters, body mass index less than 36). Other groups are currently under study. Whether INVOcell is the right tool for a patient is best determined by a reproductive endocrinologist trained in the use of the device.
Basic Fertility Treatments

Controlled Ovarian Stimulation
Controlled Ovarian Stimulation, or hyperstimulation, is a mix of medications designed to stimulate follicle development, resulting in greater egg production. It’s frequently used as the first step of in vitro fertilization (IVF).

Intracytoplasmic Sperm Injection (ICSI)
Intracytoplasmic Sperm Injection, known as ICSI, is an option for couples battling male infertility. Atlantic Reproductive has successfully completed more than 5,000 cases of this procedure over the years.

Ovarian Reserve Testing
The number of eggs a patient has available is very important when assessing fertility and possible treatments. While there is an average number of eggs, every patient is different.
Advanced Fertility Treatments

INVOcell
The INVOcell, an FDA-approved gas-permeable vaginal culture device, allows patients to incubate eggs and sperm themselves. This device decreases the cost of and increases access to fertility treatment.

IVF
One of the main fertility treatments we utilize at Atlantic Reproductive is in vitro fertilization (IVF), which involves fertilizing eggs with sperm outside the body.

IUI
Artificial insemination, also known as intrauterine insemination (IUI), is a technique that involves placing sperm inside the uterus with a catheter to achieve fertilization. Unlike IVF, artificial insemination does not require collecting eggs from the ovaries or fertilization outside the body.
