Artificial Insemination (IUI)
Intrauterine insemination (IUI), or artificial insemination, is a fertility treatment that places sperm directly into the uterus using a catheter to improve the chances of fertilization and pregnancy. IUI is a simple outpatient procedure performed at peak ovulation that enhances fertilization chances by increasing sperm-egg contact.
The goal of IUI is to increase the number of motile sperm that reach the egg, improving the likelihood of fertilization. Unlike IVF, IUI does not require the collection of eggs from the ovaries or fertilization outside of the body.
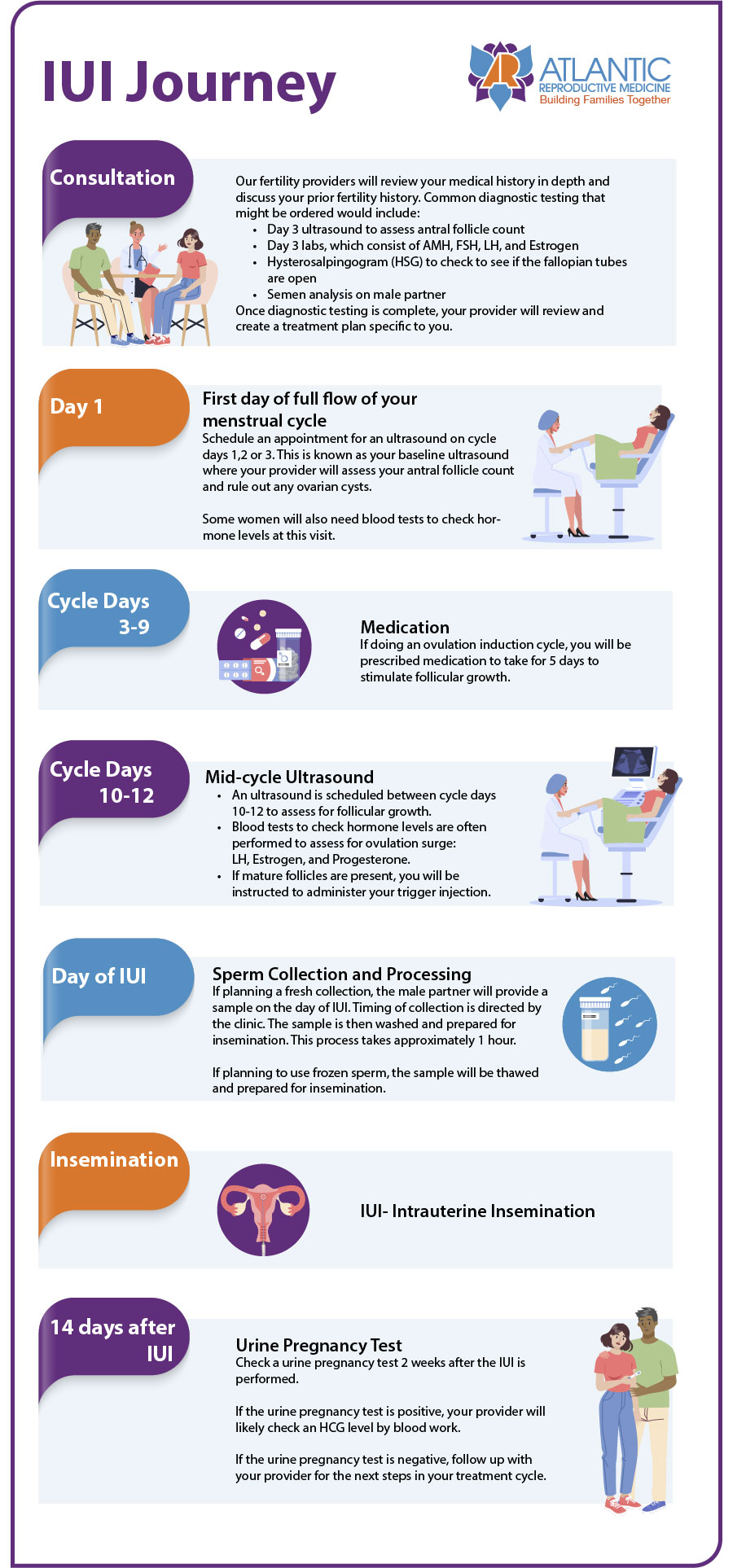
The IUI Process
- Medical Consultation – Initial assessment, labs, and tests
- Treatment Planning – Ultrasounds, medication timing, and procedure scheduling
- Sperm Preparation – Partner or donor sperm is processed to remove debris and unhealthy sperm
- Procedure – Sperm is inserted into the uterus
Expert Fertility Care in Raleigh, NC
Atlantic Reproductive provides compassionate, individualized fertility treatments, including IUI. Patients from Raleigh, Cary, Durham, Chapel Hill, Fayetteville, and beyond trust our specialists to help them grow their families.
Call us at (919) 248-8777 to schedule a consultation today to see if IUI is right for you!