No-Scalpel, No-Needle Vasectomy
What is a vasectomy?
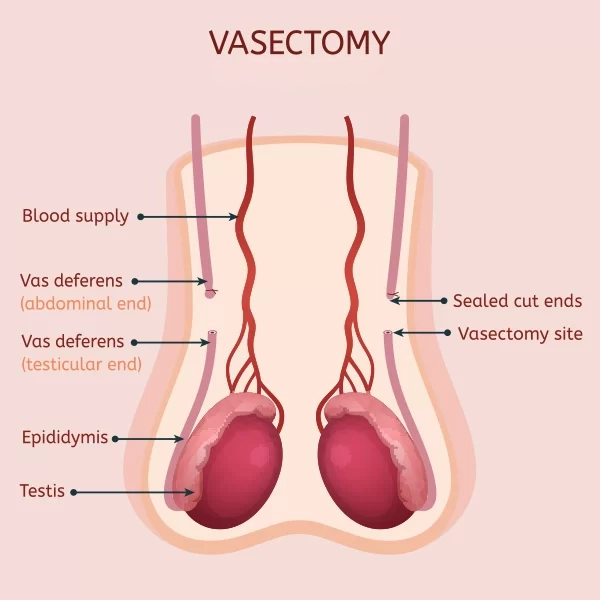
Vasectomy is a safe and permanent birth control option for males who are certain they do not want to father a child in the future. The surgical procedure is done by cutting and sealing the tubes (vas deferens) that carry sperm out of the testicles.
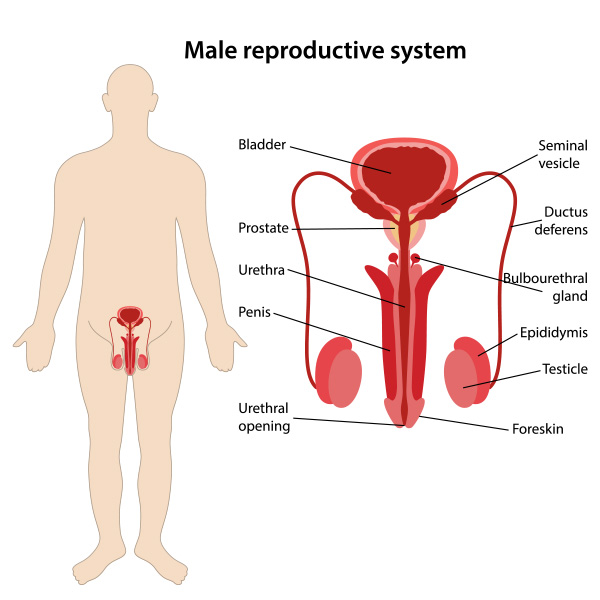
Each vas deferens is about a foot long and goes up and out of the scrotum, into the pelvis, and back around the bladder, connecting with the urethra.
Semen, or seminal fluid, comes from the prostate and the seminal vesicles. The semen mixes with the sperm from the vas deferens as they enter the urethra simultaneously during an ejaculation.
After a vasectomy, sperm will continue to swim up the vas deferens during ejaculation, but they quickly die when they reach the vasectomy site.
Are there risks with a vasectomy?
Vasectomy has a low risk of complications and is usually performed in an outpatient setting under local anesthesia. While some family medicine or general practice doctors do vasectomies, most are done by doctors specializing in the male reproductive system (urologists).
Vasectomy reversal is possible, but a vasectomy should be considered a permanent form of male birth control. Men should be certain that they do not want to father a child in the future before undergoing a vasectomy.
ON THIS PAGE
- What is a vasectomy?
- Are there risks with a vasectomy?
- How does a vasectomy compare to birth control for women?
- Unfounded concerns around sexual abilities and health after a vasectomy
- What is a no-scalpel, no-needle vasectomy?
- How is it possible to have surgery without a needle or scalpel?
- Are vasectomies reversible?
- Preparation for a vasectomy
- Recovery after a vasectomy
- The Atlantic Difference
Watch this video to learn about no-scalpel, no-needle vasectomies:
“No-scalpel, no-needle vasectomy is the least invasive form of vasectomy. My patients experience minimal pain as the anesthesia is delivered by a spray rather than a needle. Patients are able to drive themselves home after this 20-minute procedure. I am proud to be the only fellowship-trained specialist in the region offering a true no-scalpel, no-needle vasectomy. I have been doing this procedure for over 10 years and have the utmost confidence in it. I can recommend it unequivocally to my patients.” – Matt Coward, MD
The benefits of a vasectomy include the following:
- A vasectomy is close to 99.95% effective in preventing pregnancy.
- Vasectomy is an outpatient surgery with a low risk of problems or side effects.
- With a successful vasectomy, a couple no longer needs to use a condom or take other birth control steps before sex to prevent pregnancy. It does not prevent the transmission of sexually transmitted diseases.
- The cost of a vasectomy is considerably less than the cost of female tubal ligation or the long-term cost of birth control medications for women.
Why is vasectomy the simplest and easiest strategy for male fertility?
Vasectomy is the most common procedure urologists do for birth control across the United States. It is quick, has an incredibly low complication rate, and does not require general anesthesia. We offer nitrous oxide (laughing gas) during the 20-minute vasectomy for patients who feel anxious – it helps you relax while we perform this quick procedure, and its effects wear off within minutes, so you can still drive yourself home afterward. Vasectomy is the most effective male birth control available, with the lowest failure rate.
How does vasectomy compare to birth control for women?
Vasectomy is hormone-free, unlike most solutions for women who unfortunately end up bearing responsibility for a couple’s birth control more often than not. For women, an IUD (intrauterine device) is a good option that is temporary and lasts about 5 years, with failure rates around 1 percent. However, an IUD is not always well-tolerated, may have side effects, may release hormones, or may have an unacceptable failure rate for some couples.
For men, there are only two reliable forms of birth control: a condom and a vasectomy. Condoms have a high failure rate because they can break, and people do not always use them correctly.
Many men with children eventually take the responsibility of birth control off of their partners. A vasectomy requires no more than a 20-minute procedure and is usually covered by insurance plans.
Unfounded concerns around sexual abilities and health risks
Some men worry that a vasectomy can cause particular problems, but a vasectomy will not:
- Affect sexual performance. It will not affect sex drive or one’s masculinity in any way.
- Permanently damage sexual organs. There is very little risk that the testicles, penis, or any other part of the male reproductive system will be injured during surgery. In extremely rare cases, an injury to the blood supply could lead to the loss of a testicle, but again, this is extremely rare with a skilled surgeon.
- Increase risk of prostate cancer. There have been a lot of studies on this, and it is conclusive that there is no connection between vasectomies and prostate cancer.
- Cause severe pain. A feeling of minor pain and pulling can occur during surgery, but severe pain is rare. After surgery, there can be some pain, but for most men, any pain experienced is minor and goes away after a few days.
One side effect that is not uncommon is there may be a 5-10% reduction in the volume of a patient’s ejaculate, but this amount is not noticeable for most people.
What is a no-scalpel, no-needle vasectomy?
A no-scalpel vasectomy (NSV) is done by exposing the vas deferens using two specialized surgical instruments. Compared to a traditional incisional technique, NSV can result in less bleeding, hematoma, infection, and pain. It also has a shorter operative time than an incisional vasectomy.
How is it possible to conduct surgery without a needle or scalpel?
No-scalpel, no-needle vasectomy is a technique that was developed in China in the 1980s and popularized in the ’90s in the U.S. It is the least minimally invasive way of performing the procedure. While many doctors are still performing the traditional type of vasectomy, the no-needle, no-scalpel variety has many benefits.
With an NSV, the snipping of the vas deferens is done through a tiny poke-hole opening. Instead of cutting the skin, a tiny instrument pokes into the scrotal sac and spreads the sac open just a little bit. There is no actual cut on the skin and very minimal bleeding. The skin is very thin and stretchy in this region of the male body. Therefore, through this tiny hole, the surgeon can secure the vas deferens and pull it up through the skin opening to perform the vasectomy.
As the vas deferens drop back into the scrotum, the hole closes back up. No stitches are needed and there is just a minimal risk for bleeding.
Is sedation used with a no-scalpel, no-needle vasectomy?
Sedation is not necessary for the procedure, but some men choose to take an oral sedative to reduce anxiety. If you choose to take an oral sedative, you will need someone to drive you home. If not, you can drive yourself home after the procedure. It is a lot like having a dental procedure, with the primary difference being that most men have had a dental procedure and know what to expect. It is the unknown element, the uncertainty, and the sensitive area that is being worked on which can raise anxiety about a vasectomy. But there really is nothing to be anxious about.
The surgical steps of a no-scalpel, no-needle procedure
Vasectomy surgery usually takes about 20 to 30 minutes. To perform a vasectomy, your doctor will likely follow these steps:
- The area is numbed with a spray jet of a local anesthetic into the skin of the scrotum.
- With the “no-scalpel” technique, a small puncture in the scrotum is made.
- The tube that carries semen from the testicle (vas deferens) is located.
- Part of the vas deferens is withdrawn through the puncture.
- The vas deferens is cut where it has been pulled out of the scrotum.
- The vas deferens is sealed using heat (cauterizing), and surgical clips are placed. Then ends of the vas deferens are returned to the scrotum.
- With no-scalpel vasectomy, the puncture site is usually left to close on its own, and it does so relatively quickly.
What kind of pain can a patient expect with a no-scalpel, no-needle vasectomy?
Vasectomies, in general, have minimal pain. With a traditional vasectomy, the most painful part is the placement of the anesthetic with multiple needle sticks. However, no-scalpel, no-needle vasectomy is almost painless. With the no-scalpel, no-needle technique, a device sprays the anesthetic on the skin, and the patient only feels something equivalent to a mosquito bite. After several sprays on either side, a numbing feeling kicks in, and the patient stops feeling even that sensation. From that point forward, the procedure is essentially painless. In some rare instances, a patient may require additional anesthesia in the middle of the procedure.
What does recovery from a no-scalpel, no-needle vasectomy feel like?
With a no-scalpel procedure, patients only need to have a day or two of couch time at home to minimize movement. A little soreness is felt and the area can be a little swollen for two or three days. But generally speaking, the treatment is very well-tolerated. By four days after the procedure, most men can start to get back to normal activity. It takes seven to 10 days to resume physical activity and sex.
Considerations and risks with a no-scalpel, no-needle vasectomy
No-scalpel, no-needle vasectomy is a very safe procedure and the risk of complications is very low, affecting approximately only 1% of patients. It has a lower rate of complications compared to the previous conventional type of vasectomy with a scalpel.
There is a small risk of bleeding under the skin, a minor infection, or chronic discomfort. The discomfort generally gets better with time and conservative measures.
The risk of pregnancy after vasectomy is about 1 in 2,000. Since men never stop making sperm, in rare cases it is possible for sperm to make their way across the vasectomy site. With an experienced surgeon this risk is very low. Again, vasectomy has the lowest risk of failure of all forms of birth control.
A comprehensive consultation is key
The most important aspects of a vasectomy are that you are well-informed about the procedure, know it is going to be permanent, and are confident about your decision. For this reason, it is very important for you to have a consultation with a surgeon ahead of time to make sure it is the right form of birth control for you and your stage in life.

At the consultation, the surgeon might want to clarify:
- An understanding that vasectomy is permanent and that it would not be a good choice if there is any chance you might want to father a child in the future
- Whether you have children and how your partner feels about the decision,
- Other methods of birth control available for your consideration
- What vasectomy surgery and recovery involve and the rare, but possible complications
- Swelling or bruising of the scrotum
- Bleeding or a blood clot (hematoma) inside the scrotum
- Blood in your semen
- Bruising of your scrotum
- Infection of the surgery site
Rare delayed complications can include:
- Inflammation caused by leaking sperm (granuloma)
- Fluid buildup in the testicle, which can cause a dull ache that feels worse with ejaculation. There are some physicians who offer same-day vasectomies. However, studies indicate that when men have time to consider the physician’s advice, go into the office and learn about the risks and what to expect, they are much more satisfied with the procedure.
If a male has chronic testicular pain or testicular disease, he is not a good candidate for a vasectomy. For most men, a vasectomy does not cause any uncomfortable long-term side effects, and as noted earlier, serious complications are very rare.
Rare side effects right after surgery can include:
- Temporary mild pain or discomfort
- An abnormal cyst (spermatocele) that develops in the small, coiled tube located on the upper testicle that collects and transports sperm (epididymis)
- Inflammation in the scrotum caused by a fluid-filled sac (hydrocele) surrounding a testicle
- Rare chronic pain occuring in only 1% to 2% of males
- Pregnancy, in the event that the vasectomy failed; this is rare
Are vasectomies reversible?
Vasectomies are reversible, but these surgeries are almost always done because of an unexpected life event that makes a man change his mind about having children. Only about 5% of men who get vasectomies end up getting them reversed. Men who get vasectomies do so because they want a permanent solution.
Reversals are a little harder to accomplish than vasectomies. They are also more expensive and typically not covered by insurance.
A vasectomy is generally not recommended for men who are very young, single, or without children. Those are conditions that put a man at a higher risk of regret. Of course, there are exceptions.

Preparation for a vasectomy
Food and medications:
- A patient should stop taking aspirin, nonsteroidal anti-inflammatory drugs, or other blood-thinning medications at least a week before surgery. These can include over-the-counter pain medications such as ibuprofen (Advil, Motrin, others).
Pre-procedure prep:
- A shower or bath on the day of the surgery with a thorough washing of the genital area is requested.
- Men do not need to be accompanied on the day of the procedure and may drive themselves home.
Clothing and personal items
- A pair of tight-fitting underwear or an athletic supporter should be put on after the procedure to support the scrotum and minimize movement and swelling
Care after a vasectomy
Following a vasectomy, bruising, swelling, and pain can occur. It usually gets better within a few days. Instructions for recovery may include:
- Call immediately if you have signs of infection, such as blood oozing from the surgery site; a temperature of more than 100.4 F (38 C); redness; or worsening pain or swelling.
- Support the scrotum with a gauze fluff and tight-fitting underwear for at least 48 hours after the procedure
- Apply ice packs to the scrotum for the first two days.
- Full rest for 24 hours after the procedure and limited activity for a few days. After two or three days, light activity can resume, but sports, lifting, and heavy work should be avoided for two weeks or so. Overdoing it could cause pain or bleeding inside the scrotum.
- Sexual activity should be avoided for one week. An ejaculation before then can cause pain or blood in the semen.
- Birth control for sexual intercourse should be used until a semen analysis indicates that sperm are no longer present. This usually occurs after about 20-30 ejaculations and 10-12 weeks.

A vasectomy does not provide immediate protection against pregnancy
A vasectomy doesn’t provide immediate protection against pregnancy. An alternative form of birth control is needed until your doctor confirms there are no sperm in your semen. Before having unprotected sex, three months or longer must pass and ejaculation must occur 20 to 30 times or more to clear any sperm from your semen.
Most surgeons do a follow-up semen analysis 12 weeks after surgery to make certain that no sperm are present. To provide a semen sample, semen is ejaculated into a small cup.
Vasectomy will not protect sexual partners from sexually transmitted infections, such as chlamydia or HIV/AIDS. For that reason, other forms of protection such as condoms if there is risk of acquiring or transmitting a sexually transmitted infection — even after you have a vasectomy.
The Atlantic Difference
With the only fellowship-trained specialist in the region offering a true no-scalpel, no-needle vasectomy, Atlantic Reproductive Medicine is able to offer our patients the most advanced procedures for vasectomies and vasectomy reversal. If you are interested in learning more about vasectomies or any fertility or infertility issue, call us today for a consultation @ (919) 248-8777.
