Sperm Retrieval
What is Sperm Retrieval?
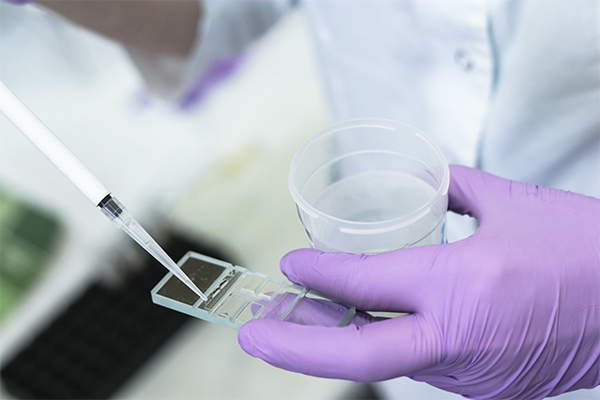
Sperm harvesting is done to find and retrieve sperm in men who want to achieve pregnancy but have no sperm in their ejaculate (azoospermia). Sperm is retrieved directly from the testis or epididymis.
There are many different techniques used for sperm retrieval, each dependent upon the patient’s specific situations as determined by an infertility specialist. Considerations may include:
- If the patient has obstruction or not
- If epididymal (coiled tube that is attached to each of the testes and where sperm mature and are stored) or testicular (male reproductive gland or gonad) sperm is preferred,
- If the couple desires to extract enough sperm for sperm banking
- If the procedure is being performed due to elevated sperm DNA fragmentation (the separation or breaking of DNA strands into pieces) or failed in-vitro fertilization (IVF).
Sperm can be extracted through procedures such as TESE, microTESE, TESA, MESA, and PESA. Most of these procedures can be performed awake in the office with local anesthesia.
ON THIS PAGE
- What is sperm retrieval?
- Where and how are sperm made?
- Retrieving sperm due to azoospermia
- Surgical procedures to extract sperm from the testes or epididymis
- What is TESE?
- What is MicroTESE?
- Rare risks with TESE and MicroTESE
- What is TESA, MESA, and PESA?
- The advantages and disadvantages of different sperm retrieval procedures
- The Atlantic Difference
Where and how are sperm made?
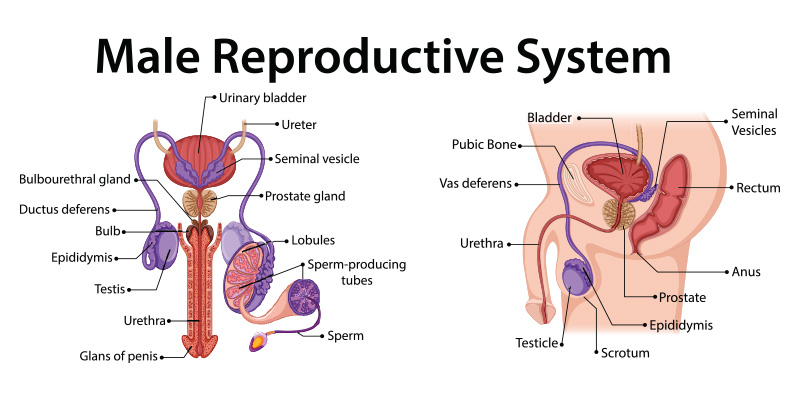
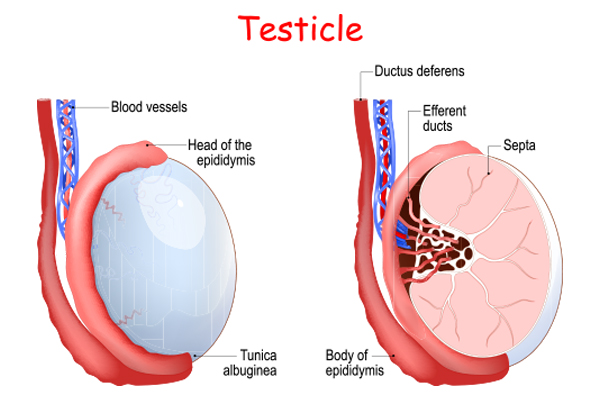
Sperm production begins in the testis in fine tubes called seminiferous tubules. In each testis, these tubes connect to a larger tube called the epididymis. The epididymis holds the sperm for a short time after production. The epididymis is connected to the vas deferens, which lead to the urethra. Sperm move through this system of tubes and are then deposited in the semen during ejaculation.
 “There are multiple techniques for sperm retrieval, each of which may be recommended in distinct situations such as blockages, low sperm production, or abnormal sperm DNA quality. We offer every type of sperm retrieval available and tailor the surgical plan to the patient’s anatomy and the couple’s overall fertility goals. Most of these procedures can be performed awake in the office with local anesthesia.” – Matt Coward, MD
“There are multiple techniques for sperm retrieval, each of which may be recommended in distinct situations such as blockages, low sperm production, or abnormal sperm DNA quality. We offer every type of sperm retrieval available and tailor the surgical plan to the patient’s anatomy and the couple’s overall fertility goals. Most of these procedures can be performed awake in the office with local anesthesia.” – Matt Coward, MD
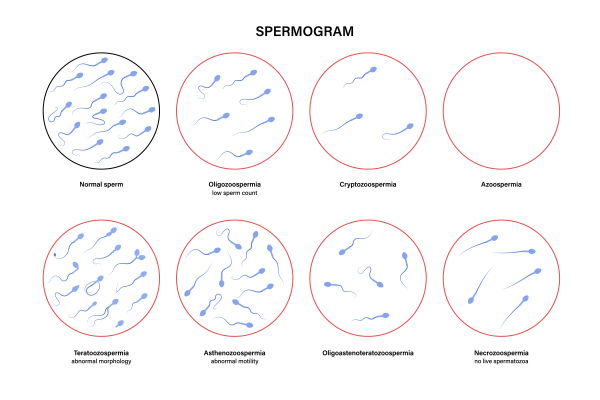
Retrieving sperm due to azoospermia
Azoospermia is a condition in which there is no sperm present in a man’s ejaculated semen. A previous vasectomy, an unsuccessful vasectomy reversal, and a blockage in the epididymis or the vas deferens are all referred to as obstructive azoospermia. Sperm is being produced in the testes, but it cannot get out of the testicles and join with semen during ejaculation.
Non-obstructive azoospermia, on the other hand, is when there is no sperm production in the seminiferous tubules of the testicles, or production is occurring at such a low level that sperm are not detectable in the ejaculate.
It is easier to harvest sperm from a man with obstructive azoospermia than from non-obstructive azoospermia. The simplest and most cost-effective procedure for obstructive azoospermia is an aspiration of sperm done under local anesthesia in a clinical office.
Retrieving sperm from a man with a testicular problem resulting in low sperm production is much more involved than obstructive azoospermia and these procedures often take several hours. The gold-standard procedure, microTESE, is performed with the aid of a surgical microscope to increase the chances of finding sperm and to minimize the amount of tissue removed from the testes.
Surgical procedures to extract sperm from the testes or epididymis
Surgical procedures are used to both diagnose what is causing azoospermia and to effectively retrieve sperm to achieve pregnancy with a partner.
Sperm retrieval procedures fall into different categories:
- Testicular sperm retrieval vs. epididymal sperm retrieval
- Open (surgical) vs. percutaneous (through the skin) retrieval
A surgeon’s decision on which type of sperm-retrieval procedure to do is based on a number of variables, including what type of sperm obstruction exists, success rate and complication considerations, if DNA fragmentation exists, and other medical factors.
Surgically removed sperm samples are suitable for in-vitro fertilization but rarely suitable for use in intrauterine insemination (IUI).
Below is a look at the various techniques used to retrieve sperm.
Retrieving sperm from the testicle: different options for different situations
TESE: Testicular sperm extraction
TESE is a procedure for getting sperm directly from the testicle. It may be the chosen treatment for sperm extraction when:
- A patient has had a vasectomy
- No sperm is found on semen analysis (azoospermia)
- In-vitro fertilization failure has occurred due to poor sperm quality
The TESE procedure is typically:
- A 45-minute procedure
- Performed in the office using numbing medication although it can be performed in an operating room using general anesthesia
- Tissue is removed from the testicle that can be frozen or used fresh for in-vitro fertilization
- Outpatient procedure; patient goes home the same day
- Successful 99% of the time, with a varied success rate depending on the individual
MicroTESE: Micro Testicular Sperm Extraction
A microsurgical testicular sperm extraction (microTESE) is another surgical option indicated for men with no sperm on semen analysis due to poor sperm production (nonobstructive azoospermia). MicroTESE is more extensive than TESE.
With this procedure:
- An operating microscope is used to find pockets of sperm production in the testicles
- If the careful searching process does not find sperm in one testicle, the other testicle will be searched
- Any sperm found can be used for in-vitro fertilization, but not IUI
- The outpatient procedure takes about 3 hours and is done in the office with numbing medication, and twilight sedation, and the patient goes home the same day
- Success rates vary between 20-70% depending on individual factors discussed during the initial consultation
Risks with TESE and MicroTESE are rare
While risks with TESE and MicroTESE are extremely rare (less than 5%), if complications do occur they may include:
- Infection
- Bleeding
- Decrease in testosterone production
- Disruption of blood flow in the testicle(s)
- Chronic pain in the testicle(s)
- Decrease in size of the testicle
The Differences between TESE and MicroTESE
TESE |
MicroTESE |
|---|---|
|
|
TESA: Testicular sperm aspiration
TESA is another procedure for sperm retrieval from the testicle for men with obstructive azoospermia due to a vasectomy or other reasons. TESA is not done as often as TESE because less sperm is retrieved and there is a higher failure rate as well as a higher complication rate compared to TESE.
TESA is, however, an easier and faster procedure. It can be done in the office with local anesthesia. A needle is inserted into the testicle to aspirate sperm. But in the cases where TESA does not provide enough tissue or sperm for IVF or intracytoplasmic sperm injection (ICSI), the surgeon will need to do an open testis biopsy to get the necessary amount or proceed to do a TESE. The scheduling of a TESA is coordinated with the partner’s egg retrieval.
Retrieving sperm from the epididymis: different options for different situations
PESA: Percutaneous Epididymal Sperm Aspiration
PESA is a procedure for getting sperm directly from the epididymis. Like TESA, PESA is a procedure for men who are having sperm retrieved for in-vitro fertilization or intracytoplasmic sperm injection (direct injection of male sperm into an egg) who have obstructive azoospermia due to a vasectomy or other reasons such as a prior infection. It can be done in an office setting with local anesthesia. Like TESA, the procedure is coordinated with the female partner’s egg retrieval.
MESA: Microsurgical Epididymal Sperm Aspiration
MESA is another sperm retrieval procedure involving the epididymis. It is performed on men who have vasal or epididymal obstruction due to a vasectomy or congenital bilateral absence of the vas deferens. MESA can be done either as a scheduled procedure or in coordination with a partner’s egg retrieval.
MESA is performed in an operating room with general anesthesia using an operating microscope. Patients typically choose to cryopreserve sperm during this procedure for future IVF/ICSI.
During MESA, the surgeon makes an incision of a single tubule. Once incised, fluid flows from the epididymal tubule and pools in the epididymal bed. The pooled fluid is then aspirated.
MESA results in a relatively large collection of mature sperm. It is the preferred method of retrieval for men with congenital bilateral absence of the vas deferens because it does not impact steroid production of the testis. Repeated aspirations can be performed, and the aspirated fluid can be used immediately or preserved with cryopreservation.
MESA and PESA are often the preferred options for men with a known epididymal obstruction like vasectomy and congenital bilateral absence of the vas deferens, a condition in which the vas deferens (tubes that carry sperm out of the testes) fail to develop properly.
What is the Difference between TESA and PESA?
PESA involves passing a fine needle through the skin into the epididymis to retrieve sperm. In contrast, TESA involves passing a fine needle through the skin into the testes to retrieve a small number of the seminiferous tubules themselves. The tubules are then searched in a lab for the presence of sperm.
How are TESA/PESA sperm used to achieve pregnancy?
Often the number of sperm retrieved through TESA or PESA is very low compared to the number usually present in ejaculate. For this reason, the retrieved sperm typically need to be used in combination with a type of in-vitro fertilization called ICSI (Intracytoplasmic sperm injection).
TESA/PESA sperm use with IVF and ICSI
Once the partner’s eggs have been collected (usually on the same day as a PESA or TESA procedure), the male’s sperm will be injected directly into the eggs (a process called intracytoplasmic sperm injection, ICSI). The fertilized eggs are then cultured for a few days in a laboratory to develop a healthy embryo that is transferred into the partner’s uterus. Often enough sperm are retrieved for some sperm to be frozen for use in future ICSI cycles if desired.
Advantages and Disadvantages of different sperm retrieval procedures
Procedure |
Acronym |
Advantages |
Disadvantages |
|---|---|---|---|
Percutaneous Techniques
|
|||
| Percutaneous epididymal sperm aspiration | PESA |
|
|
| Testicular Sperm Aspiration | TESA |
|
|
Open Techniques |
|||
| Testicular sperm extraction | TESE |
|
|
| Microsurgical epididymal sperm extraction | MESA |
|
|
Post Procedure Guidelines
Post-procedures vary somewhat depending on the sperm retrieval treatment, but typically include:
- Sperm results are available immediately
- The dressing around the scrotum can be removed in 24 hrs and a shower taken
- Work can generally be resumed in a few days
- No lifting greater than 10lbs or strenuous exercise for 2 weeks
- All skin sutures will dissolve on their own
- Intercourse can be resumed in 1 week
The Atlantic Difference
Specialists at Atlantic Reproductive Medicine can perform all types of sperm retrieval and will tailor the surgical plan to the patient’s anatomy and goals. Most of these procedures can be performed awake in the office with local anesthesia.
If you are interested in learning more about sperm retrieval, call Atlantic Reproductive Medicine today for a consultation @ (919) 248-8777.
