
Causes of Male Infertility

ON THIS PAGE
- Causes of male infertility
- Diagnosing male infertility
- Infertility tests
- What factors determine sperm health?
- What causes sperm disorders?
- The physical exam and medical history intake
- Infertility symptoms
- Varicoceles and other forms of genital tract blockage
- Azoospermia
- Infertility treatments
- Donor sperm for severe male infertility
- When to see an infertility specialist
- The Atlantic Difference
“Infertility is much more common than many people think. One in approximately eight couples experience infertility, and half of all couples experiencing infertility have a contributing male factor. For most men with infertility, we can make a diagnosis and provide multiple avenues for treatment. I am passionate about helping couples build and grow their families. I value communication and strong relationships with my patients. It would be my privilege to meet with you and discuss your goals.” – Matt Coward, MD
One out of every eight couples struggles with infertility, and for many infertile couples, there may be more than one cause. A common misconception is that an infertility problem usually lies with the female. The reality is that half of all infertile couples have a contributing male factor.
If a couple has been trying to conceive without success for one year (six months if both are over 35), there are likely to be fertility issues. It is typically helpful for both individuals to see a fertility specialist for analysis, and it is important to note that it may take a number of tests to determine the cause of infertility.
Male Factors
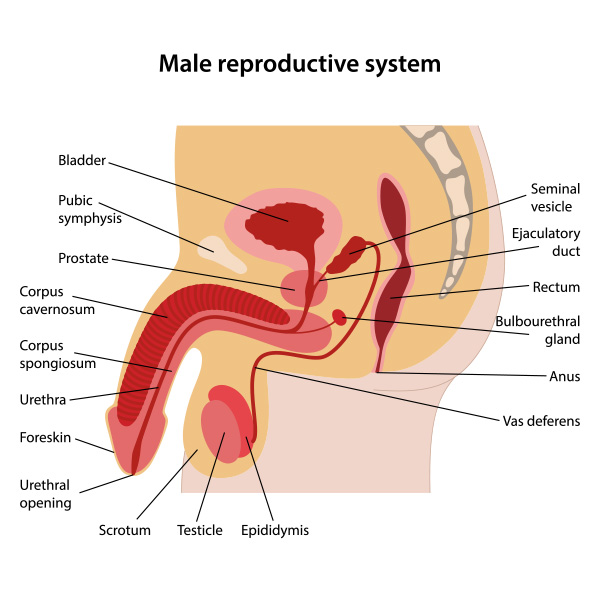
Natural male reproduction depends on creating healthy sperm that can fertilize an egg. It also depends on a male having an erection, an ejaculation, and the ability of the sperm in the ejaculate to swim to the egg.
A problem with any of these conditions can result in male infertility. As with female infertility, male infertility can have many symptoms, causes, and solutions. Luckily, several treatments are available to help with natural conception. Furthermore, if natural conception proves elusive, many other options exist for achieving conception with one’s partner.
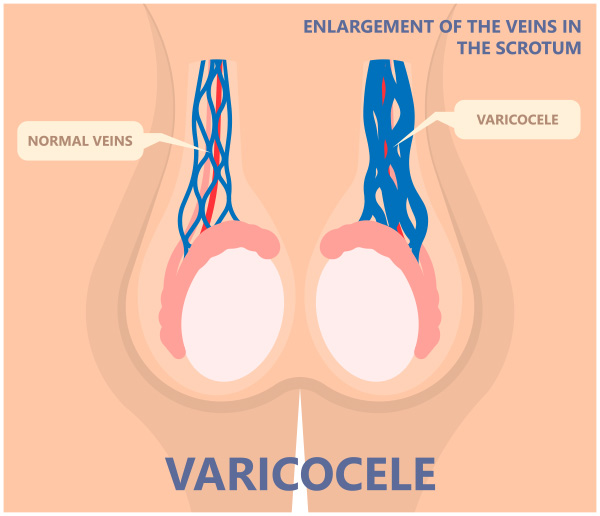
Causes of male infertility include hormonal issues, testicular production problems, varicoceles (dilation of veins in the testicles), genetic factors, and environmental and lifestyle factors.
Diagnosing Male Infertility
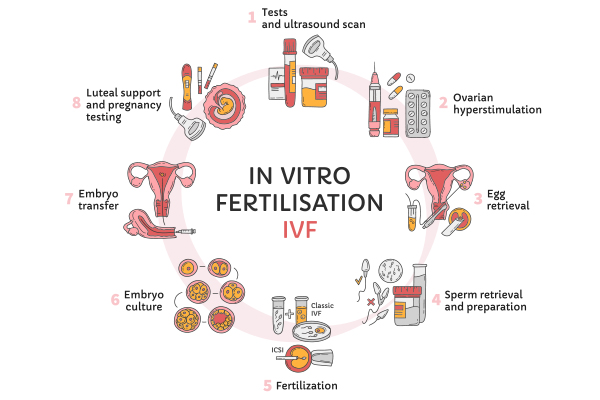
Steps for treating male infertility include identifying reproductive problems, diagnosing underlying causes, and correcting or improving medical issues that impair sperm production and sperm health. Treatments might entail lifestyle modifications, medical therapy (prescriptions), and surgery. The goal is to optimize sperm health and mobility for natural conception and/or assisted reproduction, including in vitro fertilization (IVF) and intrauterine insemination (IUI).
Watch this video to learn about male fertility, semen analysis, and a male factor evaluation:
Diagnosing Male Infertility Typically Begins with the Following:
- Semen analysis. Semen analysis examines the health of sperm under a microscope. Samples are typically obtained via masturbation by ejaculating into a special container in a private room at the doctor’s office. If you prefer an alternative method of semen collection, such as collection at home, this can be discussed with your specialist as conditions need to be optimal for obtaining a sample.
- A general physical examination and analysis of your medical history. Your doctor will examine your genitals and ask questions about inherited conditions, injuries, surgeries, chronic health problems, and any illnesses that could affect fertility. Your doctor might ask about your sexual development during puberty and past and present sexual habits.

Infertility Tests
Your fertility specialist may use some of the following tests and procedures to accurately diagnose the specific structural or medical issues that may be causing infertility:
- Scrotal ultrasound. This test uses high-frequency sound waves to capture images of the inside of your testicles and other anatomy. A scrotal ultrasound can reveal if there is a varicocele or other problems in the testicles and supporting structures.
- Transrectal ultrasound. A small, lubricated wand is inserted into your rectum to allow the specialist to examine your prostate and look for blockages of the tubes that carry semen.
- Post-ejaculation urinalysis. If your urine contains sperm, it may indicate that the sperm are traveling backward into the bladder instead of out through the penis during ejaculation (this is called retrograde ejaculation).
- Advanced semen tests. A test called DNA fragmentation may be recommended to evaluate the DNA quality of the sperm.
- Genetic tests. When sperm concentration in semen is extremely low, there might be a genetic cause. Blood tests can uncover whether there are an abnormal number of chromosomes, mismatched material from one chromosome to another, or subtle changes in the male Y chromosome, which are signs of a genetic abnormality. Genetic testing can be ordered to diagnose various congenital or inherited conditions.
- Hormone testing. Hormones produced by the pituitary gland and the testicles play a key role in sexual development and the production of sperm. Abnormalities in other hormonal or organ systems can also contribute to infertility. A blood test can measure the level of hormones and testosterone.
- Testicular biopsy. This procedure involves removing samples from the testicle to determine if sperm production is normal and whether the fertility problem is caused by a blockage or another problem with the ability of sperm to move and transport themselves effectively.
What Factors Determine the Health of Sperm?
Sperm health is evaluated on a variety of factors, including quantity, movement, and structure:
- Quantity. Quantity refers to the number of sperm in a male’s ejaculate–the semen discharged in a single ejaculate. A male is most likely to be fertile if his semen contains at least 15 million sperm per milliliter. Too little sperm in an ejaculate can make it more difficult to get pregnant because there are fewer sperm available to make the journey to an egg and succeed in fertilization.
- Movement (motility). In order to reach and fertilize an egg, sperm must move and swim through a woman’s cervix and up into the uterus and fallopian tubes. This movement is known as motility. A male is most likely to be fertile if at least 40% of sperm are able to move.
- Structure (morphology). Normal sperm have long tails and oval heads. This structural design works to propel them. While structure is not as important a factor as sperm quantity or movement, the more sperm a male has with a normal shape and structure, the more likely a male is to be fertile.
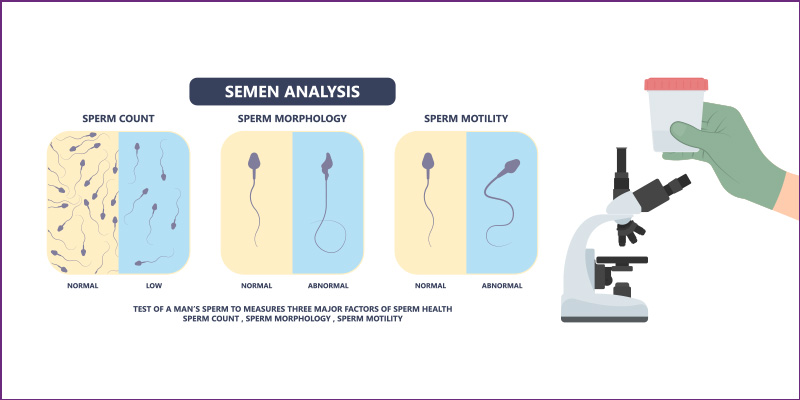
A fertility specialist will count the number of sperm in a sample, analyze its structure, and watch its movement. The laboratory will also check for signs of other problems, such as infections.
Sperm count often fluctuates significantly from one specimen to another. For this reason, several semen analysis tests may be done over a period of time to ensure accurate results.
If a male’s sperm analysis is normal, a specialist is likely to recommend thorough testing of the female partner before recommending any more male fertility tests.
What Causes Sperm Disorders?
There are many possible causes of sperm disorders, including:
- Anatomical abnormalities such as varicocele (varicose veins of the testicle) or history of an undescended testicle(s)
- Environmental and lifestyle factors such as heavy use of tobacco, alcohol, steroids, marijuana, or exposure to toxins
- Hormone or pituitary gland problems
- Use of testosterone or workout supplements
- Genetic disorders such as being a carrier for cystic fibrosis or having an extra or misplaced portion of a chromosome
- Medical problems such as a history of cancer or uncontrolled diabetes
- Serious childhood illnesses
- Childhood surgeries, including hernia repair or testicular injuries
- Kidney or liver infections, other infections, inflammatory conditions,
- Vasectomy
The Physical Exam and Medical History Intake
A physical exam and medical history intake can also uncover potential issues such as premature ejaculation or structural issues such as erectile dysfunction or blockage problems that may cause male infertility.
Infertility Symptoms
Infertility symptoms may include:
- Pain, swelling, or a lump in the testicle or groin areas
- Problems with sexual function, such as difficulty with ejaculation, small volumes of fluid ejaculated, difficulty maintaining an erection (erectile dysfunction), or lack of interest in sex
- Urinary, bladder, or prostate symptoms include urinary frequency, burning, incontinence, or difficulty voiding.
- Abnormal breast growth (gynecomastia)
- Decreased facial or body hair
- Difficulty sleeping
- Depression or significant stress
- Being older than 45 years of age
Varicoceles and Other Forms of Blockage in the Genital Tract
Blockage in the genital tract might result from a genetic or birth defect, an infection or inflammation from a sexually transmitted disease, scar tissue from surgery, or dilated veins in the scrotum (varicoceles).
Testicles of different sizes, a complaint of tenderness or pain, and other factors may be signs of varicoceles and dilation of the veins within the scrotum. Varicocele is a common condition, affecting 15-20% of all males, and the main cause of male infertility. It is the most common cause of an abnormal semen analysis and is usually readily diagnosable during a physical exam.
A physical examination with a reproductive urologist is necessary to confirm a diagnosis. Occasionally, an ultrasound test provides more details of the testicular veins.
Varicocele surgery performed by a reproductive urologist (doctor specializing in male reproductive organs) is an effective treatment for varicoceles. The specialist clips or ties off the testicle veins, causing the symptoms. The surgery stops blood from flowing through those veins, and soon other veins accommodate the blood flow.
Azoospermia
The complete absence of sperm in the ejaculate is called azoospermia. The cause of azoospermia can be obstructive or non-obstructive. Obstructive azoospermia may be treatable with reconstructive surgery, while non-obstructive azoospermia typically requires sperm retrieval and in-vitro fertilization (IVF).
One frequently used procedure for non-obstructive azoospermia is micro-TESE, in which a reproductive urologist finds and retrieves sperm using an operating microscope.
Watch this video to learn about the in-office microsurgery procedures Dr. Coward performs at Atlantic Reproductive Medicine:
Treatments for Male Infertility
There are many treatments for male infertility, depending on the specific cause. They include:
- Surgery. Surgery can repair dilated varicose veins in the scrotum (varicocele repair), which can often improve the quality of sperm. An obstructed vas deferens can be repaired to correct infertility. Additionally, sperm retrieval procedures can help men with severely abnormal semen quality, those who are azoospermic (no sperm in the ejaculate), and those with disorders of erection or ejaculation. In men with a history of vasectomy, a vasectomy reversal or sperm retrieval can be considered.
- Hormone medications and treatments. A fertility specialist may recommend hormone medications if infertility is caused by low levels of certain hormones or problems with how hormones are used by the body. Hormonal disorders may be caused by a problem in how the pituitary gland and testes interact, which affects how sperm develop. Treatments might include hormone modulators such as clomiphene citrate or gonadotropin therapy.
- Treating infections. Antibiotic treatment might cure an infection of the reproductive tract. This does not always restore fertility, but in some cases, it does.
- Lifestyle adjustments. A patient’s risk factors will be assessed, and recommendations for healthier life choices might be made, including tobacco cessation, decreased alcohol consumption, avoidance of testosterone and workout supplements, improved sleep, weight loss, and improved diet.
- Treatments for sexual intercourse problems. Medication or counseling can help improve fertility in conditions such as premature ejaculation or erectile dysfunction.
- Assisted reproductive technology (ART). ART treatments involve obtaining sperm through normal ejaculation, surgical extraction, or from donor individuals. The sperm can then be inserted into the female genital tract or used in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) to achieve pregnancy.
- Artificial insemination. This treatment, also known as intrauterine insemination (IUI), inserts a well-timed, highly concentrated sample of healthy sperm into your partner’s uterus with the hope that the sperm will make their way to the fallopian tubes.
- IVF and ICSI. In vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) is assisted reproduction where fertilization and embryo development occurs in the embryology laboratory. The sperm is collected, and a high-quality sperm is selected and injected into your partner’s egg to create an embryo that can be transferred back into the partner’s uterus.
Donor Sperm is an Option for Severe Male Infertility
In some cases, male fertility problems cannot be treated despite the best technologies and medications. At that point, a fertility specialist might suggest that a male and his female partner consider using sperm from a donor.
Anonymous donor sperm can be purchased from a sperm bank and shipped to a fertility clinic for intrauterine insemination (IUI) or in-vitro fertilization (IVF).
When to see an Infertility Doctor
You should consider seeing an infertility specialist if you and your partner have been unable to conceive after a year of unprotected sex and you have any of the following conditions:
- Erection or ejaculation problems, other problems with sexual function, or a low sex drive
- Pain, discomfort, or a lump or swelling in the testicle area
- A groin, testicle, penis, or scrotum surgery in your medical history
- A history of testicle, prostate, or sexual problems
- You are 45 years of age or older
The Atlantic Difference
Every fertility situation is unique. Every male situation is unique. At Atlantic Reproductive Medicine, we aim to provide the highest possible level of personalized fertility care. We offer the best fertility services across all needs and all procedures. Contact us today to set up a consultation with our male infertility specialist @ (919) 248-8777
Male Fertility Treatments

Causes of Male Infertilty
A common misconception is that an infertility problem usually lies with the female. The reality is that half of all infertile couples have a contributing male factor.

Vasectomy Reversal
Vasectomy reversal is a surgical procedure to undo a vasectomy and when done by a skilled surgeon it is successful on most men.

MicroTESE
Microsurgical testicular sperm extraction (microTESE) retrieves sperm from the seminiferous tubules of a male’s testes in men with non-obstructive azoospermia.
No-Scalpel, No-Needle Vasectomy
No–scalpel, no-needle vasectomy is the least invasive form of vasectomy, a safe and effective form of birth control for males who are confident they do not want to father a child in the future.

Semen Analysis
Semen analysis evaluates the quality and volume of a sperm in semen. It is one of the first steps to detect male infertility issues.

Azoospermia & Abnormal Semen Quality
Azoospermia is the absence of sperm in the ejaculate. Abnormal semen quality in ejaculate refers to quality issues with sperm in the semen that can make the sperm unable to achieve fertilization of an egg.

Varicocele
A varicocele is a dilated vein within the scrotum which holds and protects the testicles. It can occur in one or both testicles and can cause male infertility.

Ejaculatory Dysfunction
Ejaculatory dysfunction is among the most common sexual disorders but there are many solutions, including medications, assistive neurostimulatory methods, and surgical sperm retrieval.

Sperm Selection
Sperm selection can separate highly motile, normal sperm from those of lower quality which is critical for fertility treatments such as intrauterine insemination (IUI), in vitro fertilization (IVF), or intracytoplasmic sperm injection (ICSI).

Sperm Retrieval
Sperm retrieval (harvesting) is done to find and retrieve sperm from the testis or epididymis in men who want to achieve pregnancy but have no sperm in their ejaculate.
