Infertility is a challenging and common issue that affects both men and women. One out of every eight couples struggle with infertility.
If a couple has been trying to conceive without success for one year (six months if both are over age 35), both individuals should seek a fertility specialist for analysis. For many couples, there may be more than one cause.
Half of all infertile couples have a contributing male factor. In approximately 20% of infertile couples, the male factor is the only cause of the couple’s difficulty conceiving. A surprising statistic is that approximately 10% of couples dealing with infertility have a male partner with azoospermia (the semen sample contains no sperm at all).
Natural male reproduction depends on a male 1) creating healthy sperm that can fertilize an egg 2) being able to have an erection and ejaculate and 3) the sperm must be able to swim to the egg in the fallopian tube. A problem with any of these conditions can result in male infertility. However, just as there can be many symptoms and causes of male infertility, there are also many solutions.
When it comes to male infertility, recognizing the signs early on is crucial for seeking timely medical assistance.
In this blog, we’ll explore male infertility and answer these questions:
- How Common is Male Infertility?
- What Causes Male Infertility?
- Common Signs of Infertility in Men
- How to Tell if You are an Infertile Male
- Can you Fix Male Infertility?
- Can Male Infertility be Prevented?
How Common is Male Infertility?
According to the World Health Organization (WHO), approximately 7% of men worldwide face infertility-related challenges. This percentage has been gradually increasing, making it a significant health concern worldwide and resulting in more and more couples needing fertility treatments to build their families.
What Causes Male Infertility?
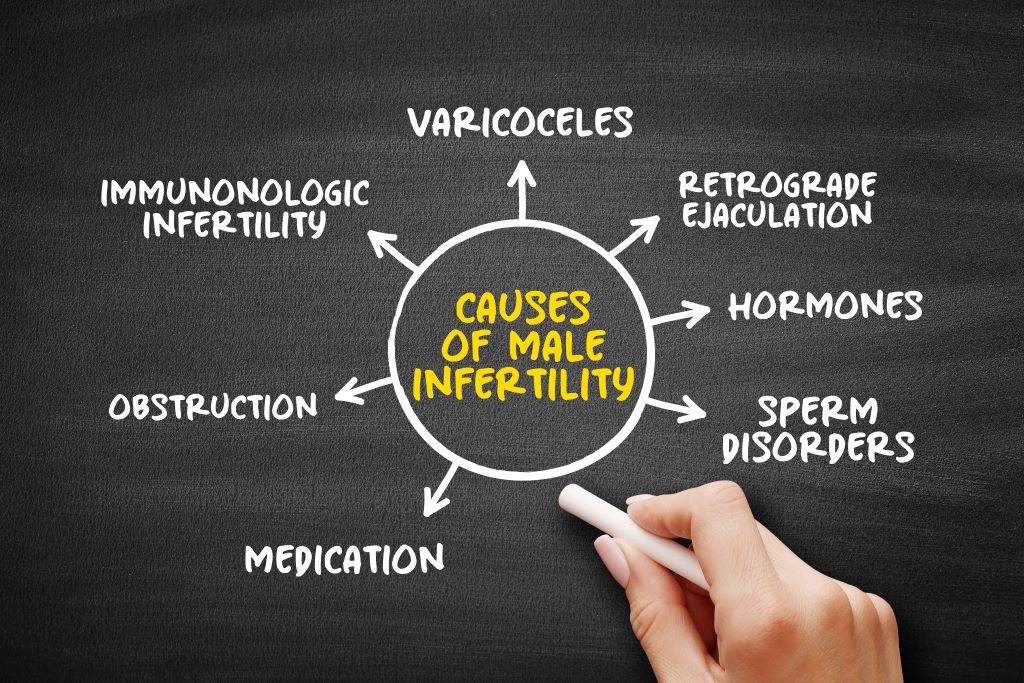
Understanding the root causes of male infertility is essential for effective intervention. Various factors contribute to fertility issues in men, ranging from lifestyle choices to medical conditions. Some common causes include:
- Sperm Disorders: Problems with sperm production, motility, or morphology can lead to infertility.
- Varicocele: A varicose vein in the testicles can impact sperm production and quality. Most varicoceles are very treatable in the hands of an experienced microsurgeon.
- Hormonal Imbalances: Disruptions in hormonal levels, such as low testosterone, can affect fertility.
- Genetic Factors: Inherited conditions or genetic abnormalities may contribute to male infertility.
- Environmental Factors: Exposure to toxins like tobacco, alcohol, or cannabis; heat; radiation, or even certain chemicals can harm sperm production. These exposures are more common than we think and can occur at home, in the workplace, or in the diet.
Common Signs of Infertility in Men
Recognizing the signs of male infertility is crucial for early diagnosis and intervention. Some common indicators include:
- Most often, there are no symptoms other than difficulty conceiving with your partner for more than 12 months.
- Recurrent Miscarriage: Three or more miscarriages should prompt evaluations of both the female partner and the male partner.
- Changes in Sexual Function: Difficulty maintaining an erection or ejaculating
- Pain or Swelling: Discomfort or swelling in the testicular area, such as a lump in the testicle or groin areas
- Issues with Ejaculation: Premature ejaculation or other ejaculatory problems such as difficulty maintaining an erection, small volumes of fluid ejaculated
- Low Sperm Count: A semen analysis showing a lower-than-normal sperm count
- Urinary, bladder, or prostate symptoms, such as urinary frequency, burning, incontinence, or difficulty voiding
- Decreased facial or body hair or abnormal breast growth
- Depression, difficulty sleeping, lack of interest in sex
- Being older than 45 years of age
How to Tell if You are an Infertile Male
If you suspect you may be experiencing infertility issues, it is important to consult with a fertility specialist. Helpful diagnostic tests may include a physical exam, semen analysis, hormonal testing, and imaging studies.

Physical Exam
During a physical examination, your fertility specialist will examine your genitals and ask questions about possible inherited conditions, past injuries, surgeries, any chronic health problems and any illness that could affect fertility. Your doctor might ask you about your sexual development during puberty and past and present sexual habits.
Semen Analysis
Semen analysis examines the health of sperm under a microscope. Semen samples are typically obtained via masturbation and ejaculation into a special container.


Hormonal Testing
Hormonal testing is an important component of the diagnostic process for male infertility as hormones regulate reproductive function and can significantly impact sperm production, maturation, and overall fertility.
Hormonal testing for male infertility is typically conducted through blood tests. These tests are usually performed in the morning, as hormone levels can vary throughout the day. The results of hormonal testing, combined with a thorough medical history and other diagnostic evaluations (such as semen analysis), help healthcare professionals identify the specific causes of male infertility.
Here are the hormones commonly tested in the evaluation of male infertility:
- Testosterone: Testosterone is the primary male sex hormone, and its levels are essential for normal sperm production (spermatogenesis). Testosterone is made by the testicles. Low testosterone levels can be associated with male infertility.
- Luteinizing Hormone (LH): LH is responsible for stimulating the production of testosterone in the testicles. Abnormal high levels of LH can indicate issues with the testicles’ ability to produce testosterone, and low LH can indicate pituitary signaling problems or suppression by external sources of testosterone or androgens.
- Follicle-Stimulating Hormone (FSH): FSH is crucial for spermatogenesis. Elevated FSH levels may suggest a problem with the testicles’ ability to produce sperm, and low FSH can indicate pituitary signaling problems or suppression by external sources of testosterone or androgens.
- Prolactin: Prolactin is a hormone associated with the production of breast milk. Elevated levels in men may indicate a pituitary gland disorder that can affect reproductive hormones.
- Estradiol: While higher levels of estrogen are typically associated with females, small amounts are present in males. Elevated levels of estradiol in men can affect fertility and may be associated with certain medical conditions.
Once hormonal imbalances are identified, appropriate interventions, such as hormone or other targeted treatments, may be recommended to address the underlying issues and improve fertility.
Imaging Studies
Your fertility specialist may want to do a scrotal ultrasound to accurately diagnose the specific structural or medical issues that may be causing infertility.
A scrotal ultrasound uses high-frequency sound waves to capture images of the inside of your testicles and other anatomy. A scrotal ultrasound can reveal if there is a varicocele or other problems in the testicles and supporting structures.
Can You Fix Male Infertility?
The good news is that most cases of male infertility are treatable. Depending on the cause, treatments may include: lifestyle changes, medication, or surgical interventions. The goal with these treatments is to optimize sperm health and mobility for natural conception and/or assisted reproduction, including in vitro fertilization (IVF) or intrauterine insemination (IUI).
Can Male Infertility Be Prevented?

While not all causes of male infertility are preventable, adopting a healthy lifestyle can significantly reduce the risk. Key preventive measures include:
- Maintaining a Healthy Weight: Obesity can negatively impact fertility, so maintaining a healthy weight is crucial.
- Avoiding Excessive Heat: Prolonged exposure to high temperatures, such as hot baths or saunas, can affect sperm production. Occupational heat exposures should also be considered.
- Limiting Exposure to Toxins: Minimizing exposure to environmental and occupational toxins and chemicals is essential for reproductive health. Men should avoid excessive alcohol use, tobacco, and cannabis or marijuana.
- Managing Stress: Chronic stress can impact hormonal balance, so adopting stress management techniques is beneficial.
- Diet: A heart-healthy diet rich with antioxidants from fresh fruits and vegetables is the best diet for sperm production. Men should avoid fried and processed foods as well as excessive red meat.
- Exercise: A routine of getting cardiovascular exercise for 30 minutes per day has been shown to reduce stress and maintain healthy weight, and is associated with better semen parameters.
- Sleep: Sleeping at least 7 hours per night is ideal for maintaining a healthy body. Sleep disruptions from snoring, sleep apnea, insomnia, or intermittent night shift work can negatively impact male reproductive function.
Being aware of the signs, understanding the prevalence, and taking preventive measures are essential in addressing male infertility. Seeking timely medical advice and exploring available treatments with a highly experienced male fertility specialist can significantly improve the chances of overcoming fertility challenges and achieving the dream of parenthood.
Atlantic Reproductive Medicine has one of the most highly-trained and experienced male fertility experts in the world. Dr. Matt Coward, a North Carolina native, is a renowned urologic microsurgeon specializing in treating male fertility. He is one of the only reproductive urologists in the region offering microsurgical male fertility procedures within the collaborative setting of an in vitro fertilization (IVF) practice. Having male and female specialists working in the same clinic gives a couple the confidence that their care will be comprehensive and well coordinated. Atlantic Reproductive Medicine offers the latest treatment advancements, technologies, and testing with a state-of-the-art lab….all in one clinic.
Travel to Atlantic Reproductive Medicine is convenient, and the Raleigh area is inviting. The office is only ten minutes from Raleigh-Durham International Airport and is centered in the Research Triangle, known for its biotech companies and three top-tier universities (UNC, Duke and NC State). World-class hotels, museums, restaurants, walking trails, and more, make visiting the Raleigh area enjoyable.

